Previous
Next

Welcome Statement
Hi Everyone – Welcome to our new Website!
It is focused on the promoting Primary Healthcare (PHC), Education
and Support among to the disadvantaged and the hard-to-reach rural
people in Developing Countries like Uganda. In these regions, majority
of people still live under high levels of poverty, poor health and very
low or no education at all. It is usually the women groups, mothers and babies, children, the elderly and those with living with disabilities (the disabled) who are found to be most economically disadvantaged, socially marginalized and therefore most vulnerable. Also increasingly included today are those living with new and special, non-communicable but treatable illnesses, diseases and ailments – collectively called Non-Communicable Diseases (NCDs) – that such people in these communities are forced to live with through their lives.
Project Name and Status
The name of the Health Project is Teresa Mobile Health KliniK Services (TemoheKs) – locally-grown rural and community-based Charity and NGO – personally initiated by me (Mr Okanya Kokas) – to provide the people of Mukongoro Sub-county, Kumi district, Teso region and in the deep rural part of Eastern Uganda (my birth place) – with basic Primary + Specialist Healthcare, Education and Support services that have continued to be greatly lacking yet very badly needed.
Project Aim and Purpose
Main aim and purpose of Teresa Mobile Health KliniK Services (TemoheKs) is to create a reliable sustainable outreach public health program through which basic Primary Healthcare, Education and Support services are regularly provided to the disadvantaged groups of people living in such these remote isolations (and in almost total neglect) – the rural region of Mukongoro Sub-county. Mr Okanya Kokas is an original-born of this area and even though he now lives in Australia (full citizen), he has been working on this project since 2007 with quiet determination to make it happen. For instance – in February 2015 he shipped – with help of some “great Australian friends” – the 1st steel container of medical equipment and materials – all the way from Brisbane (Australia) to the actual site in Uganda – where many activities especially in form of preliminary construction had already began.
Brand Name
Brand name and design shown above was the one found most fitting for Teresa Mobile Health KliniK Services (TemoheKs) Project. It points directly on the purpose for which the project had been created – reflecting also on the kind of activities and services to be fossed upon – ie centrally the Basic Rural Primary and Specialist Healthcare, Education and Support. The Brand also geographically identifies the area location (for the project) as the rural regions – which in the case of the underdeveloped countries such as Uganda – provide the home for the majority (80-90%) of the populations in concern. Communities in these regions still live under high levels of poverty, poor health, low income and education – thus remaining largely “undeveloped, marginalized and underprivileged” – in terms of community development services such as basic primary health + education. They stay isolated, “almost forgotten” and quite vulnerable to “outside forces” – especially as in relation to health and diseases.
Other distinct features common to rural populations in developing countries include:
- general lack in basic forms of community development – hence poorly served with (government) services such as good infrastructure, education, health, transport etc
- low productivity – hence lack of incomes for investment on development (as already identified above)
- prevalent food shortages (hunger) and poor feeding (including nutrition)
- non-urbanised and distances away from town areas where community development activities and services exist – thus rendering them not easily accessible, unaffordable and even unsustainable.
Further aspects of these communities include:
- tendency to remain restricted (out there) in the countryside areas – with many staying homeless, lonely and not poorly fed
- in direct reference to the project – these people have very limited access to affordable, close and sustainable health services – even in form of basic Primary and Specialist HealthCare, Education and Support
- death-rates among these groups of people are high – many often left to rely on themselves, local traditional practices and relatives for support
- the most vulnerable groups among these people are dominated by women, mothers and babies, children, the elderly and disabled – including also those forced to live with “ particular” ailments and in-born infirmities that can be easily treated
The mobile primary healthcare services therefore to be introduced through the TemoheKs Project shall be a new strategy to further address the health concerns of the people in these disadvantaged communities – with focus on providing a much more reliable, mobile outreach operation that also ensures access to even previously “untouchable” areas. Pre-project surveys on the health features and conditions of these groups of people also reflect and suggest messages that fit in with the actual primary health concerns, needs and interests.
Logo and Slogan
Project logo clearly shows the target groups (or clients) that the services shall mostly be directed to – i.e. :
- women, mothers and babies
- children
- the aging and elderly
- the disabled and
- those with “special” or “hidden” non-communicable illnesses and diseases (NCDs)
Its Slogan – Every Human Life has Value – reflects directly on the (human) feelings and value the project holds for people – hence their health and well-being.

Timelines and Head Office
2007 marks the actual initiation of the project – with official launch on 15-04-2015 (see Developments and Progress webpage). This is considered as the start of Phase I – when able work (especially notable construction) began taking place. A number of house-blocks are now at mid and near-completion stages (see description on the Developments and Progress webpage) – with Block A – for instance – being the first one of the blocks to be completed and already in full use today as both the project Head Office and also interim Maternity Unit (photo below).
Focus Areas:
Areas of focus for TemoheKs project are:
- Primary Healthcare (PHC)
- Specialist Medical Services (SMS)
- Smart Healthcare Services (SHS)
(i) Primary Healthcare (PHC)
What is Primary Healthcare?
World Health Organization (WHO) defines Primary Healthcare (PHC) as –
“socially appropriate, universally accessible, scientifically sound first level care provided by a suitably trained workforce supported by integrated referral systems and in a way that gives priority to those most in need, maximizing community and individual self-reliance and participation and involving collaboration with other sectors”.
By its mode of operation – especially the model “mobile and outreach”, location (remote and rural regions) and target clientele (the marginalised and often left-out) – the focus of Teresa Mobile Health KliniK Services (TemoheKs) project shall definitely be Primary Health Care practices, Support and Education. It must also be universally accessible and affordable, scientifically sound; and with first level care and support services – just as in the urban areas – and provided to these groups under socially appropriate methods and by organized suitably trained workforce supported by integrated referral systems and indeed in “a way that gives priority to those most in need, maximizing community and individual self-reliance and participation and involving collaboration with other sectors”.
The 5 (five) focus areas of achievements shall be:
- universal coverage – reduction and exclusion of health and social disparities in the community
- needs and expectations-based health services – organized around people’s needs and expectations
- integrated health public policy – considers all sectors of public life
- leadership – pursuing collaborative models of policy and dialogue
- public participation – involving all and other stakeholders in the health processes.
NB:
With a general saying that “Good Primary Health Care keeps away the doctor”, the best and majority of Primary Health Care practices, Support and Education services and activities usually occur outside the hospital – thus justifying the need for “effective Primary Health Care and Support to avoid the hospital”
Activities and services in the practice of Primary Health Care practices, Support and Education usually include – promotion of basic health, prevention of illness, care of the sick, and general development of the community. For Teresa Mobile Health KliniK Services (TemoheKs) project, criteria in the Primary Health Care practices, Support and Education activities and services shall therefore involve:
- establishment of a health system that is comprehensive and coordinating with everyone in the community
- ensuring equitable distribution of basic health care for everyone
- whole community participation
- local capacity building – ie developing a Local or Community Health Workforce in the community itself to undertake responsibility for the people’s own health
- application of technology that is appropriate to the level of the community (integrating culture and language)
- multi-sectional approach (holistic)
(ii) Specialist Medical Services (SMS)
NCDs are becoming the world’s biggest killers – accounting for nearly 70 percent of all deaths. But many of these non-communicable diseases – such as cancer, cardiovascular disease, chronic respiratory diseases, and diabetes etc can be prevented and the suffering from their effects, reduced – under what is today known as Specialist Medical Services (SMS). This concept was initiated by a small group of founding medical professionals on a passion for providing the highest quality of personalized care to patients – through seeking the best (possible) multidisciplinary information on which to base medical decisions of quality care.
Together with advanced technology and state-of-the art facilities available today, they try to apply a broad range of multidisciplinary, consultative and diagnostic services – critically investigating the health care of patients concerning the range of diseases and illnesses appearing today.
A wide range of specialist health professionals have therefore evolved in different areas of health needs – providing services to groups of “forgotten” people – particularly in rural communities (of under-developed countries) – most are forced to live with but may not be aware of – such as bone and heart-related diseases, nutrition-related illnesses of diabetes.
In most of these countries – staggering numbers of children are born with congenital facial deformities and they suffer with them their whole lives. Impacts of such afflictions can include: – physical and psychological pain, shame, isolation and also guilt with sadness as they grow.
Deformed children also feel different from the peers; and in many cases they are ridiculed and ostracized from society. Their lives become lonely and without hope. They may also become plagued by chronic infections, at which point the deformity can become dangerous – and sometimes fatal.
Medical Specialists have therefore become increasingly important for early detection and protection, management, control and treatment – including even education and research.
These experts (often volunteers) do provide early checks, intervention and prevention – thus discovering these diseases early – such as common pandemics like HIV and Aids, lung infections (especially TB), whooping cough and flu and various other diarrhoeal infections (like ebola and cholera) – just as a few prominent examples. These visiting or travelling Specialists and Experts can deal with and also collect samples and data to take away for (better) analysis overseas for further diagnosis and prescriptions.
(iii) Smart Healthcare Services (SHS)
In our Primary Health Care practices, Support and Education, people must also be encouraged to practice what is called – Smart Health approach in their health practices. They should target both Physical and Mental fitness – which is keeping both the body and mind (brain) active. (In most cases, people tend to emphasize on one and forget the other – especially Mental Fitness).
Mental health or fitness is about keeping the brain active and making one feel young. It is about having or retaining a good cognitive reserve – ie always keeping the connection between neurons active. At times it can be a difference between Brain Stimulation and Dementia!
Some obvious strategies include to keep the brain active (mental health and fitness) include:
- avoiding excessive lifestyles that degrade the brain activity – such as excessive drinking and drugs
- keeping the mind/brain occupied/ busy with good stuff and activities like –
- keeping (good) company
- read books
- x-word puzzles
- socializing with friends (join a club)
- knitting
- go and watch games/sports
- keep learning (eg computers, new languages etc)
Also:
- mentoring and volunteering
- do caring activities (for people, pets etc)
- have a garden (to look after plants etc)
NB: Six (6) other easier and best ways to routinely exercise the brain – (ie ways to continually reset the brain) are:
- meditation
- play – helps to (psychologically) exercise the brain
- sleep – allows the brain to rest and re-set
- also to deal with stress and fatigue
- 4-6 hrs a night
- physical excursive – 3 hrs a week is enough (30min a day)
- socialise –
- mixing with people
- mingling
- networking
- following and changing routine ( as in food, sleep, exercise, rest etc)
- will power – very important to retain ability to make decisions and choices – eg
- picking the right time to do things
- what to choose
- how to do it
- decision to say NO!
- etc
But all these “brain/mental” stimulation exercises should be done together with good Primary Healthcare and Support practices
Project area and location
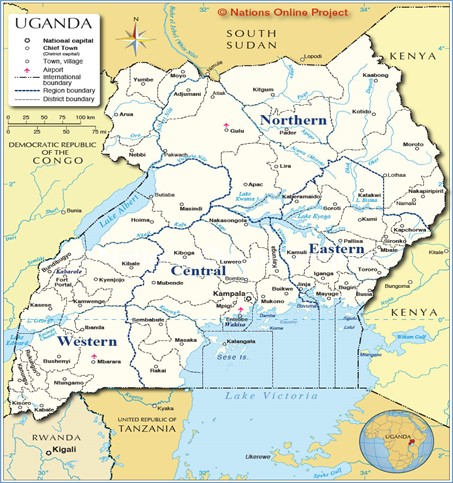
Teresa Mobile Health KliniK Services (TemoheKs) project is a home-grown NGO and also Charity – and is being operated in the Eastern part of Uganda; in the remote and rural Sub-county of Mukongoro in the district of Kumi; Teso region (see map). Estimated total area is 2,848.1 sq. km, resident 2015 census population of 54,400 (26,546 females and 27,854 males) – most of them surviving on sedentary subsistence existence.
In 2015, the Sub-county has been sub-divided into 16 (sixteen) administrative parts (or parishes) – as listed in the inset – with the name of the pilot village called – Omerein–Odeidei; a distance of nearly 400 kms from Kampala; the Capital City of Uganda. The Health Centre itself is known by the name of Ostrolia-1; already with a number of existing properties with purpose-built rooms.

AFRICA – UGANDA
Eastern Region
Teso District and County, Mukongoro sub-county Odeidei Parish
Apaade-Omerein village _______
350 + from Kampala (Capital City)
-KUMI DISTRICT
Area – 1,055sq.km
Population (2010)-GR 4.3%
M 113,600
F 120,200
Sub-counties –7
Parishes-83
Villages 170
Perspectives and Legacies
Perspective (i) – Mr Okanya Kokas
Mr Okanya was born in 1949, grew up and spent my early life in the same village of Kakures (Mukongoro, Kumi, Teso) – never leaving it for long spaces of time – except for temporary periods to attend boarding schools and eventually University. For Junior Secondary he attended Ngora High School – 22 miles away from home and the best one at the time then (1961-62); then for Senior Secondary School went to Tororo College – some 100 miles to the East.
In 1967, he passed and joined Sir Samuel Baker School (PongDwong) for Higher School Secondary – in Gulu; this time 250 miles to the extreme north of the country and near the Sudan. From here Mr Okanya finally entered Makerere University in Kampala – the only one then and located in the Capital City of the country and 400 miles to the South of his birth place.
But what had always of great memory to Mr Okanya was the privilege to always go back home (to the village) during all the holiday breaks – to stay with the family and relatives. To him that was what instilled to his heart “love for the village and his people” – such that even today with the Australian passport that he does thankfully hold, a greater part of his heart and mind still rests with great passion for these people of the (rural) Sub-county of Mukongoro. And for this he has always struggled to pay periodic visits every 3-4 years (since his arrival to Australia 1985) – back to the place he still calls HOME and retains an ancestral connection; while Australia remains his country.
Uganda got its political independence from Britain in 1962 and all that children such as Mr Okanya and his generation knew about the country’s health services then was what happened in the rural area where he lived. There was a famous ”Ford”…………. van run almost entirely by Christian Missionaries. mobile outreach clinics services –In the case of Uganda the 2 (two) major and competing Christian religious denominations were The Anglican Church and The Catholic Church – all based in Europe. Each Missionary Group set up rural outposts from where they operated their religious emissaries whilst providing minimal health and services and basic elementary schooling.
According to Okanya, his father (Tukei by name) when allocating his children to school distributed them (quite randomly) between the two Missionary Churches and with no gender consideration. Mr Okanya was placed into the Primary School run by Anglicans – better called Native Anglican Church (NAC). It was the Anglican Church also who ran regular weekly health visitations to the outpost (Mukongoro) and a small 2-roomed semi-permanent building with red-iron roof and sharing the school compound …………….was used to administer the health services.
It was every Tuesday that a white Bedford box-ambulance with a team headed by a white missionary (usually a male doctor – sometimes a lady) came in with 2-3 black Nursing Aids (and Midwifery Trainees) to conduct open-air checks, registrations, interviews, examinations including basic on-the-spot information education and counselling especially on pregnancy and maternity care, motherhood in general and infant care for the women of the area
Once a girl or woman registered a pregnancy, she was monitored regularly throughout the medical visits (ie every Tuesday) until delivery time. She also got immediately enrolled into the Anglican Church and was expected to participate in all related activities.
Regular on-the-spot information, education and counselling continued (during the visits) and with a strong demand (instructions) to have the baby delivered at the Anglican Maternity Centre – located at a place called Ngora (25 miles away) and largely for safe delivery and early mother and infant care plus monitoring. To the school children these Tuesday visitations were quite a weekly spectacle not to miss – to see all levels of pregnant women or with infants turning up on the day for inspections, treatment or registering as new cases. The health visits were well rehearsed across all families in the region and with the help of the local chiefs no one (once registered) ever missed them.
All due cases (or found near to deliver) during the visit were right away referred to the Maternity Centre) and the carers (usually the husbands) instructed to immediately take the wives (often on bicycles). Also the operating hours during visitations were from 9-00am to 3.00pm (all through lunch) so clients carried their own packed lunches (or were followed with supplies by husbands as they came to return them home).
This is the historical perspective that I wish to highlight to signify in particular the planned operation of Teresa Mobile Health Klinik Services project – to provide the outreach service for the communities left out in the rural areas.
The mobile health services offered by the missionary agencies (although inadequate) served for general and basic Primary Health Care and support and have remain significant to us today. Principle focus included in the main – maternity and child care advisory/counselling service plus general hygiene. Today’s health structures (despite under our own African leadership) are of no match at all in many aspects – especially for the rural areas.
Many health Centres are non-functional with chronic lack of even the basic medical services, including drugs and skilled personnel. Drugs can instead be easily purchased at “black market” prices and in flee-shops that operate as “shadow”clinics”! And with the income-poor, weak, old or disabled who cannot afford to pay or walk the distance, they have to learn to do without – even the basic and vital (health) services. Expecting mothers have re-learned to give birth at home; with higher risk rates of child and maternity complications and tragic losses. People in rural places like Mukongoro have been driven (once again) to travel the long distances like Ngora – in search of the vital maternity, childcare and treatment services – or revert to traditional health methods that a few still remember. To me therefore, whether for simply medical or maternity services, general treatment or information and support for even the ageing and disabled people, there is increasing need each day for the restoration of such services that can be provided through Mobile Health Outreach Clinics of the same kind – hence the motivation for the this Teresa Mobile Health Klinik Services project There are many trained but unemployed medics (including retired and experienced) that would willingly serve in the project
Perspective (ii) – Mary Teresa Abuut
Mary Teresa Abuut was Mr Okanya’s first wife for ten years but unfortunately died at an early and premature age 27 leaving 3 little boys – the youngest under 2 years. She suffered excessive haemorrhage without available blood for transfusion. This occurred in a government public hospital and she was pregnant with their fourth child – a baby girl that they had very much longed for. Delivery was also to be in same week that Teresa was to also graduate as a full Nurse and Mid-wife (3-years course). The maternity complications she witnessed could very easily have been prevented.
This occurred in a government public hospital and she was pregnant with their fourth child – a baby girl that they had very much longed for. Delivery was also to be in same week that Teresa was to also graduate as a full Nurse and Mid-wife (3-years course). The maternity complications she witnessed could very easily have been prevented.
The couple therefore missed out on a double celebration – a new baby-girl that they had longed for so long and also and of the course successful completion of the life-time course. Instead the baby was cut out dead – largely exhaustion for both mother and mother. Teresa herself died a few days later – unstoppable bleeding due to lack right type of blood!.
Today, many women and mothers still die like Teresa in most underdeveloped countries such as Uganda – and commonly from lack of Basic Primary Maternity Care – with an estimation of 30-37 a day!. Teresa Mobile Health Klinik Services project (Temoheks ) – has therefore been partly set up in Teresa’s memory principally to cut down or stop completely the loss of lives of mothers and babies at birth – largely due to lack of proper primary maternity health care. Improper Primary Healthcare and Support greatly lacks among vulnerable groups living in rural areas -where such services are both too costly and unavailable. Major victims are also usually – the marginalised in the society – mostly women and mothers, growing children, old and ageing people, those with disabilities and also with special (but treatable) illnesses and diseases. Basically Teresa died – like many still today – due to lack of basic Primary Maternity Health Care services. Teresa Mobile Health Clinik Services project is therefore rightfully dedicated to her – hence its name
Project area and Justification
Mukongoro Sub-county (Etem in Ateso – the ethnic language) and where the project is being set up remains administered under the District of Kumi and Eartern part of Uganda (see map). Mukongoro Sub-county has a total of 16 parishes (itela); each parish further divided into sub-parishes or wards (ironya) – which then make the lowest rung of government representation at rural or village level. Services and activities of the Clinic shall are received at ward or village level where the target groups live. The village or ward in which the project is based is called – Odeidei-Omerein – some 400 kms from Kampala; Country’s Capital City (see map) and therefore deep in the rural area.
The District of Kumi was also pointed out (in the 2009 census) as one of the two poorest districts in Eastern Uganda – along with Katakwi to the North – both being largely due to the cattle rustling which continued to hit the region; worsened by the 20+ years of civil and military insurgency from the Lord’s Resistance Army (LRA) Sudanese-based army rebels – right from 1986. It has therefore been very difficult for the communities in both the project area and whole District to break through the impacts of such disturbances – poverty and underdevelopment – further aggravated by forced homelessness in the so-called Internally Displaced People-Camps (IDPCs) for now almost 20+ years’ stretch. Throughout this period, people have also been kept virtually on-the run; with appalling consequences of heavy life and property losses; food and income insecurities. The most affected groups – women, mothers and babies, children, girls and boys, and also the disabled and the elderly have been left displaced, vulnerable and weak – and not also forgetting the effect of HIV and Aids epidemic which at this time of turmoil went on uncontrolled thus disseminating further the populace.
In all cases, social, economic, health and political conditions operating all this time have never been favourable; with seemingly little attention from government. Poverty, Health services and Education in particular have been left seriously wanting; and never at all meeting the people’s essential requirements; mostly the needy users in the Sub-county and the District. In terms of development and modernization therefore, districts like Kumi; and in particular deeper rural sub-county areas like Mukongoro have remained in state of stagnation and for most part total retrogression. Majority of people rely heavily on their own physical efforts and energies to farm locally just to live (subsistence and peasantry). With such extreme poor levels of development, poor education and inability to even access the most essential medical and health support services, it has been almost impossible for the people in these areas to lead the equivalent of what would be called (in the western countries) “basic standards of living”. Health services have therefore been left seriously wanting – both in terms of accessibility and affordability – since once again – most people live on no sources of dependable income!
Then, finally without education of “any useful quality” at all, majority of people (in the District) have been left at extremely high levels of illiteracy – too low to meet the people’s essential requirements in general public life and employment. There is therefore much need for total rehabilitation (or repair) of not only the economic and social livelihood of such communities but placing greater focus on the front-line support services for development – which include basic health and education.
Introducing TemoheKs program (in a rural region such as Mukongoro) with its multi-pronged approach of targeted activities and services to the community shall help to address the urgent needs of these people as outlined above in “ a great positive way”. In terms of health in particular, the project with its own mobile targeted service system – shall create the medical primary healthcare infrastructure that has always lacked – to manage related shortages in client’s needs and interests. Issues such as endemic lack in necessary drugs, active health workers or basic medical sundries and equipment and access to basic medical information shall be ameliorated – since the mobile clinic service shall travel to the clients to work with them at their own site locations. Importantly, there is also a strong plan in the project’s operation to directly engage with the community in activities such as education, training and counselling – seminars, workshops, information sessions etc – to directly benefit the people to uplift their skills, knowledge and capacities in understanding Primary Health Care to raise the quality of their lives and generate support for the project’s sustainability. Indeed if successfully implemented, TemoheKs project shall definitely be “one big step” in helping to address the urgent Health Care needs for this particular rural region of Mukongoro – and also be front-line in poverty alleviation
General medical statistics – Uganda 2015
COUNTRY HEALTH PROFILES (Uganda 2010)
Major demographics
Source: WHO World Bank UNESCO, Country Database (2010)
-
Population Growth
- 1960 …. 7m
- 1980 …. 12.5m
- 2000 … 24m
- 2015 … 37m
- 2030 … 46m
- 2050 … 91m
-
Life Expectancy
- 1980 … Male 42 … Female 45
- 1200 … Male 48 … Female51
- 2020 … Male 54 … Female 57
- 2050 … Male 62 … Female 68+
-
Incomes + General Welfare (GDP = U$ 600-800)
- 57% Live in dwellings with 1 room
- 44% Live in 2+ rooms (mostly towns)
- 52% Neither employed / in education
- 58% Do not add value to govt/debt
-
Top 10 causes of death(killers) in Uganda
- HIV and Aids
- Influenza +Pneumonia
- Diarrhoeal infections
- Maternal Conditions + Abortions
- Malaria
- Strokes + Coronary Conditions
- Traffic Accidents + Violence
- Violence + Injuries
- Lung-related (tuberculosis)
- Lung-related (tuberculosis)
35 Wars
-
Top 10 Killer Cancers and World Ratings
- Cervical Cancers (WR=11)
- Breast Cancers
- Oesophageal Cancers
- Prostate Cancers
- Stomach Cancers
- Liver Cancers
- Lymphomas Cancers
- Colon-rectum Cancers
- Oral Cancers
- Ovarian Cancers
Project Scope and Overview
Primary Health Care plays an important role in disease prevention efforts in both the developed and developing world. In the later, this is predominantly through local health systems and non-governmental organizations – like TemoheKs. WHO is the international agency that coordinates and acts on global public health issues whilst most countries have their own government public health systems, sometimes known as Departments of Health – to respond to domestic health issues. In Uganda for example, Primary Health Care and Support is managed under the Ministry of Health and is expected to be responsible for public health, emergency preparedness and response, infectious and chronic disease control and prevention. The public health systems and health care facilities are owned by Government.
But in the developing countries there often exists great disparity in access to health care and public health initiatives in comparison to between developed nations. In the developing world, public health infrastructures are still forming. There are often not enough trained health workers or monetary resources to provide even a basic level of medical care and disease prevention. As a result, a large majority of disease and mortality in the developing world results from and contributes to extreme poverty. For example, many African governments spend less than US$10 per person per year on health care, while, in the United States, the Federal Government spent approximately US$4,500 per capital in 2000 (World Health Organization report 2003).
But expenditures on healthcare should not be confused with spending on public health. Public health measures may not generally be considered “health care” in the strictest sense. For example, mandating the use of seat belts in cars can save countless lives and contribute to the health of a population, but typically money spent enforcing this rule would not count as money spent on health care!
So in the case of Teresa Mobile Health Klinik Services (TemoheKs) project, the main hope and intention is to provide the rural people of the designated region – Mukongoro sub-county – and in particular the underprivileged, marginalized, and disadvantaged – almost forgotten – women groups in general, mothers and babies, children, the elderly, the disabled and also those with hidden “infirmities and ailments” that can be easily treated with the help of Specialists – with opportunities to lift their lives through better Primary Health Care practices and Support services
Vision
In the ultimate, the visionary hope of Teresa Mobile Health Klinik Services (TemoheKs) is –“transformation of the rural communities in the identified project area (Sub-County of Mukongoro) to those that are healthy and in particular – always enjoying (sustainable) sound and high level Primary Health Care and Support services that are easily accessible and affordable to everyone”. By focusing mainly on the most disadvantaged, marginalized and vulnerable, the people in these isolated communities also get equal opportunities for quality life – for instance longer life-spans (as those in the urban areas) and upholding the project’s slogan of – “Every Human Life Has Value”.
The other visionary hope is “a community with capacity to practice basic and new (modern) Primary Health Care and Support practices on their own – and applying strategies that are appropriately integrated with the existing traditions – for better, accepted and sustained community health and wellbeing”.
Mission
Missionary activities and services of Teresa Mobile Health Klinik Servives shall be directed mostly towards fulfilment of the project’s objectives, goals and vision. In general, they will be to improve levels of basic health in the target communities and groups – starting with or mostly through promotion of Primary Health Care practices, Support and Education. Priority shall always be to the disenfranchised groups left out without such services.
The Clinic key tasks shall therefore involve the following actions and services:
- improving Primary Health Care practices, Support and Education among the general community – but in particular the “unreachable” rural women in general, mothers and babies in particular; children, the elderly and the disabled
- arranging for treatment services (through Specialist Doctors) to people (seemingly) forgotten in the rural areas with special illnesses and diseases that are often never given any medical attention – but left to suffer through most parts or all of their lives
- establishing a Primary Health Care Centre as “Hub” for providing the necessary Primary Health Care practices, Support and Education services to the general community – but specifically the identified client groups
- establishing a mobile health service medical infrastructure for delivering Primary Health Care, Support and Education + treatment services to the unreachable (remote) locations – where most of the target client groups are situated
- having a stand-by Clinic ambulance – for movement of patients and routine visitations to the rural treatment sites to deliver on-site Primary Health Care practices, Support and Education
- developing an effective basic Primary Health Care practices, Support and Education information package and program for promoting understandable Primary Health Care and Support practices and services to the community and target client groups
- promoting basic Primary Health Care practices, Support and Education services awareness and consciousness among the community (ie educating, counselling, training and positively influencing people towards new mindsets of better health – general benefits of the TemoheKs project
- encouraging the target clients ( including general public) to actively participate in and support the Clinic and project – by being involved in its activities and services; actual volunteering and sharing information with others to improve community health
- encouraging the community to develop supportive attitudes towards weaker members of the community – especially vulnerability in groups like women, mothers and babies, children, the elderly and the disabled.
- specifically to work to change and improve the lives of the disadvantaged people in society such as those with disabilities or with “hidden infirmities” that can be treated by Specialist Doctors – through arrangements to visit the project from time to time– thus giving these people new quality living
- better focus and management of human health care all through years of life – ie planning strategies of good living right from good mothering and child care, through adulthood to old age; including disability care if it occurs.
- extension of the TemoheKs (its activities and services) to other areas and communities of need and demand – especially neighbouring regions and even districts
- creating synergistic opportunities from the project – such as local employment local labour, volunteers and youth.
- The youth especially can get opportunities to further upgrade their skills to earn better incomes
- promote activities, knowledge and awareness for healthy living in community in general – such as good feeding and nutrition, fitness exercises, good company, regular monitoring of health etc
- also working in liaison with local health agencies and organizations (including government) for better community health – to be passed on the community and the client groups.
Objectives
- Focus of a public health intervention – particularly in practicing basic Primary Health Care, Support and Education (as in Teresa Mobile Health Klinik Services Project) – is to prevent and manage diseases, injuries and other health conditions through surveillance of cases and the promotion of healthy behaviours in communities and environments. Many diseases are preventable through simple, non-medical methods.
For example, Research has shown that:
- the simple act of hand washing with soap can prevent many contagious diseases
- in other cases, treating a disease or controlling a pathogen can be vital to preventing its spread to others, such as during an outbreak of infectious disease, or contamination of food or water supplies.
- also public health communications programs, vaccination programs, and distribution of condoms are examples of common public health measures.
Measures such as these have contributed greatly to the health of populations and increases in life expectancy. Key objectives in the services of Teresa Mobile Health Klinik Services shall therefore include:
- understanding the communities in the project area and identifying groups that are most disadvantaged and greatly suffering from lack of basic Primary Health Care, Support and Education
- targeting the identified groups (and the general community itself) with improved basic Primary Health Care, Support and Education services
- providing the target client groups with services, support and information they require that relate to basic Primary Health Care, Support and Education
- active mobilisation, participation and involvement of the target groups with the program – to directly benefit from the activities and services provided
- targeting people with “special and hidden” illnesses and diseases – often left helpless and yet can be treated and living in these rural communities – with Medical Specialists visits
- raising the capacities among the people in the rural community – on basic understanding and appreciation of the program (basic Primary Health Care, Support and Education); its significance/value to people and need to support it (sustainability)
- support for the project and its activities and services – as a means of fighting poverty in such rural communities – because through targeted health education, counselling and capacity building, people will improve their perspectives of life; productivity and production levels – hence better living from higher incomes. Example – We can fight poverty by creating positive awareness of impact of such pandemics as HIV/AIDS on individual performance and economic activities like farming and even capacity to do work (being productive).
- creation of employment opportunities for some members of the community in activities relating to the various arms of the project – such as counseling etc. Some of them (especially the youth) can earn sponsorships to higher places training/skilling – hence access to better jobs and incomes!
- effectively engage with the target groups – especially in information sharing, communication mechanisms – for networking and dissemination – on matters regarding community primary health care; and also encouraging them to actively be involved in activities like education, counseling and simple training workshops being offered through the project.
- improved sense of community Primary Health Care and Support; security and confidence in the TemoheaKs project and its services to the people.
- lifting of living standards among the rural people in the project area in general (+ the adjoining regions) – through good results, popularity and credible performance.
- to strengthen project advocacy and lobbying at client and community level as a strategy for linking communities to supportive organizations – especially those related to community health including government.
Goals and Outcomes
Teresa Mobile Health Klinik Servives (TemoheKs) sees itself as a very ambitious project with range of anticipated outcomes – both immediate and direct whilst others shall be indirect and also long-term.
The obvious major goal shall always be the successful transformation of the marginalized and “un-served” rural population of the identified Mukongoro Sub-county – into a region whose community also enjoys high sustained standards of basic Primary Health Care, Support and Education services – with easy access and affordability – and people themselves actively involved in its operation
Other goals – also with synergistic impacts shall include:
- a healthy community that practices Primary Health Care, Support and Education across the identified groups and with capacity of people themselves to take better care of their own Good health leads to higher productivity.
- availability in the community of basic intervention, prevention and protection, management and control of Primary Health Care and Support services for themselves – including basic education and understanding of what is required to sustain needed levels of health.
- effective understanding (and support) of the need for data collection for further analysis and research to discover better ways to deal better with and sustain community Primary Health Care, Support and Education.
- dramatically change and improve Primary Health Care, Support and Education among the target client groups – which include the rural women, mothers and babies, children, the old, the disabled and those with special illnesses.
- effective information access, communication and sharing by and across the target groups and entire community of the project area – for sustained understanding of Primary Health Care practices, Support and Education.
- effective knowledge and information sharing and understanding by and across the target groups and entire community of the project area on general Primary Health Care, Support and Education – including how poverty reduction is linked to the project.
- effective use of information, communication, access and networking for greatly affected communities to develop capacity for sustainable economic growth (improved incomes and profits) as a result of keeping healthy and fit.
- extended demand for project (other regions) as true evidence of its success.
- introduction of new lifestyle health-related activities such as community fitness and weight-loss etc as a result of successful Primary Health Care, Support and Education program.
- popularisation of the program, expansion and upgrade of the program to other regions – including establishing Health Centres at new locations due to its high and positive performance.
- finally – acknowledgement and recognition of TemoheKs’ model of practice and operation as an effective mobile and outreach facility – in general disease-control and management cycle – ie detection, management and control, prevention and protection and community Primary Health Care, Support and Education (in particular).
Project inspiration (Drivers)
Major drivers for Teresa Mobile Health Klinik Services project have mostly been:
- legacies behind the project
- traditional family responsibility – as the 1st born – care for others
- life in exile (nearly 30 years) and strong pressure to return home … to do something!
- observing the “state” of living and health among my people (as reported above) – during the regular (personal visits) with home
- significance of Primary Health Care and level it is practised in the rural regions – life spans, death
- rates, general livelihoods etc
- belief that Primary Health Care in such areas can be improved and I can do something about it”
- sudden personal scare from hidden illnesses – suspected cancer!
- full retirement and finding something (more meaningful to life) to do with all available time
- support and encouragement from friends
- shared legacy – for Teresa and Family (read below)
Contact Us
Contact us in Uganda
Contact us in Australia
Head Offices
Teresa Mobile Health Klinik Services (TemoheKs) shall operate its Head Office at the following locations.
Email:
info@teresamobilehealthservices.com
Website:
www.teresamobilehealthservices.com
Attention:
Mr Okanya Kokas
Ostrolia 1, Apaade-Omerein, Mukongoro, Kumi, Teso,
Uganda
P O Box 359, Kumi, Teso ,
Uganda
Phone:
+256 773 390 218
Attention:
Mr Okanya Kokas
68 Brighton Road, Highgate Hill, 4101
Brisbane Queensland, Australia
Phone:
+61 470 420 366

Copyright © 2013 Teresa Mobile Health Klinik Services. All Rights reserved.